Chapter 246-16 WAC
Last Update: 11/30/15STANDARDS OF PROFESSIONAL CONDUCT
WAC Sections
| HTMLPDF | 246-16-010 | Purpose of chapter. |
| HTMLPDF | 246-16-020 | Definitions. |
SEXUAL MISCONDUCT | ||
| HTMLPDF | 246-16-100 | Sexual misconduct. |
MANDATORY REPORTING | ||
| HTMLPDF | 246-16-200 | Mandatory reporting—Intent. |
| HTMLPDF | 246-16-210 | Mandatory reporting—Definitions. |
| HTMLPDF | 246-16-220 | Mandatory reporting—How and when to report. |
| HTMLPDF | 246-16-230 | Mandatory reporting—License holder self reports. |
| HTMLPDF | 246-16-235 | Mandatory reporting—License holder reporting other license holders. |
| HTMLPDF | 246-16-240 | Mandatory reporting—Reports by professional liability insurance carriers. |
| HTMLPDF | 246-16-245 | Mandatory reporting—Reports by health care institutions. |
| HTMLPDF | 246-16-250 | Mandatory reporting—Reports by health service contractors and disability insurers. |
| HTMLPDF | 246-16-255 | Mandatory reporting—Reports by professional review organizations. |
| HTMLPDF | 246-16-260 | Mandatory reporting—Reports by courts. |
| HTMLPDF | 246-16-265 | Mandatory reporting—Reports by state and federal agencies. |
| HTMLPDF | 246-16-270 | Mandatory reporting—Reports by employers of license holders. |
SANCTIONS | ||
| HTMLPDF | 246-16-800 | Sanctions—General provisions. |
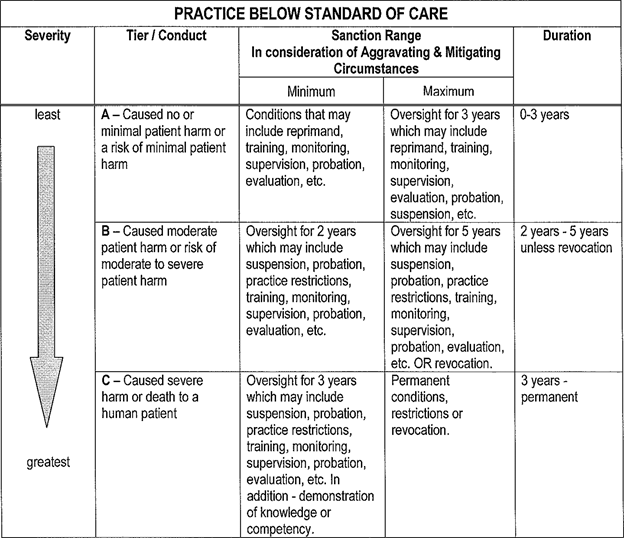
| HTMLPDF | 246-16-810 | Sanction schedule—Practice below standard of care. |
| HTMLPDF | 246-16-820 | Sanction schedule—Sexual misconduct or contact. |
| HTMLPDF | 246-16-830 | Sanction schedule—Abuse—Physical and emotional. |
| HTMLPDF | 246-16-840 | Sanction schedule—Diversion of controlled substances or legend drugs. |
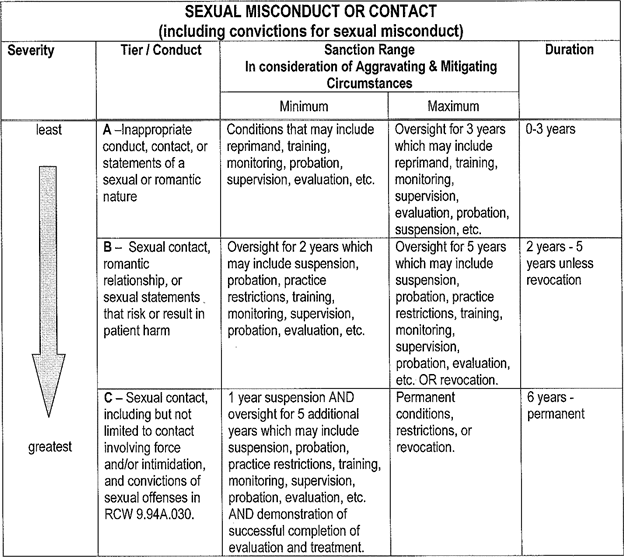
| HTMLPDF | 246-16-850 | Sanction schedule—Substance abuse. |
| HTMLPDF | 246-16-860 | Sanction schedule—Criminal convictions. |
| HTMLPDF | 246-16-890 | Sanctions—Aggravating and mitigating factors. |
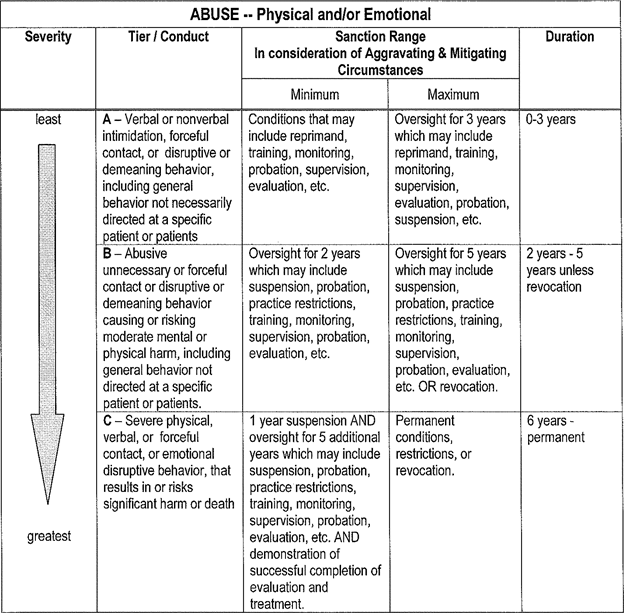
PDF246-16-010
Purpose of chapter.
The rules in this chapter define certain acts of unprofessional conduct for health care providers under the jurisdiction of the secretary of the department of health as provided in RCW 18.130.040 (2)(a) including persons licensed or certified by the secretary under chapter 18.73 RCW or RCW 18.71.205. The rules also provide for sanctions. The secretary may adopt rules applicable to specific professions under RCW 18.130.040(2). These rules also serve as model rules for the disciplining authorities listed in RCW 18.130.040 (2)(b).
[Statutory Authority: RCW 18.130.050 (1), (12) and 18.130.180. WSR 06-18-045, § 246-16-010, filed 8/30/06, effective 9/30/06.]
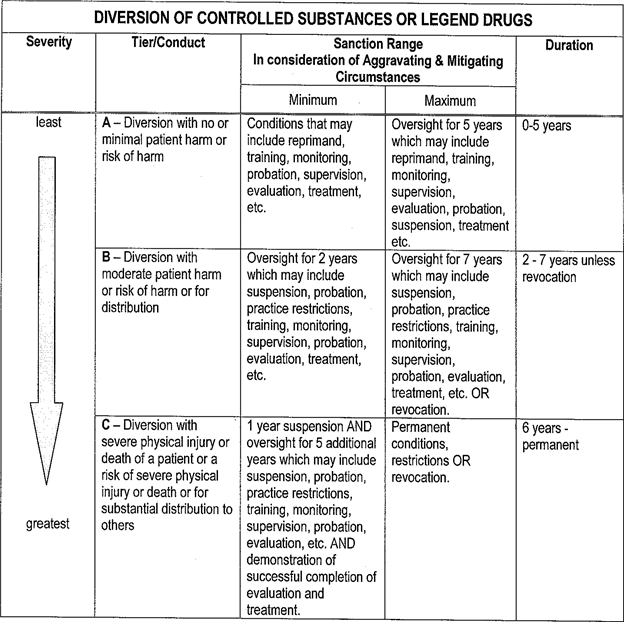
PDF246-16-020
Definitions.
(1) "Health care information" means any information, whether oral or recorded in any form or medium that identifies or can readily be associated with the identity of, and relates to the health care of, a patient or client.
(2) "Health care provider" means an individual applying for a credential or credentialed in a profession listed in RCW 18.130.040 (2)(a).
(3) "Key party" means immediate family members and others who would be reasonably expected to play a significant role in the health care decisions of the patient or client and includes, but is not limited to, the spouse, domestic partner, sibling, parent, child, guardian and person authorized to make health care decisions of the patient or client.
(4) "Legitimate health care purpose" means activities for examination, diagnosis, treatment, and personal care of patients or clients, including palliative care, as consistent with community standards of practice for the profession. The activity must be within the scope of practice of the health care provider.
(5) "Patient" or "client" means an individual who receives health care from a health care provider.
[Statutory Authority: RCW 18.130.050 (1), (12) and 18.130.180. WSR 06-18-045, § 246-16-020, filed 8/30/06, effective 9/30/06.]
SEXUAL MISCONDUCT
PDF246-16-100
Sexual misconduct.
(1) A health care provider shall not engage, or attempt to engage, in sexual misconduct with a current patient, client, or key party, inside or outside the health care setting. Sexual misconduct shall constitute grounds for disciplinary action. Sexual misconduct includes but is not limited to:
(a) Sexual intercourse;
(b) Touching the breasts, genitals, anus or any sexualized body part except as consistent with accepted community standards of practice for examination, diagnosis and treatment and within the health care practitioner's scope of practice;
(c) Rubbing against a patient or client or key party for sexual gratification;
(d) Kissing;
(e) Hugging, touching, fondling or caressing of a romantic or sexual nature;
(f) Examination of or touching genitals without using gloves;
(g) Not allowing a patient or client privacy to dress or undress except as may be necessary in emergencies or custodial situations;
(h) Not providing the patient or client a gown or draping except as may be necessary in emergencies;
(i) Dressing or undressing in the presence of the patient, client or key party;
(j) Removing patient or client's clothing or gown or draping without consent, emergent medical necessity or being in a custodial setting;
(k) Encouraging masturbation or other sex act in the presence of the health care provider;
(l) Masturbation or other sex act by the health care provider in the presence of the patient, client or key party;
(m) Suggesting or discussing the possibility of a dating, sexual or romantic relationship after the professional relationship ends;
(n) Terminating a professional relationship for the purpose of dating or pursuing a romantic or sexual relationship;
(o) Soliciting a date with a patient, client or key party;
(p) Discussing the sexual history, preferences or fantasies of the health care provider;
(q) Any behavior, gestures, or expressions that may reasonably be interpreted as seductive or sexual;
(r) Making statements regarding the patient, client or key party's body, appearance, sexual history, or sexual orientation other than for legitimate health care purposes;
(s) Sexually demeaning behavior including any verbal or physical contact which may reasonably be interpreted as demeaning, humiliating, embarrassing, threatening or harming a patient, client or key party;
(t) Photographing or filming the body or any body part or pose of a patient, client, or key party, other than for legitimate health care purposes; and
(u) Showing a patient, client or key party sexually explicit photographs, other than for legitimate health care purposes.
(2) Sexual misconduct also includes sexual contact with any person involving force, intimidation, or lack of consent; or a conviction of a sex offense as defined in RCW 9.94A.030.
(3) A health care provider shall not:
(a) Offer to provide health care services in exchange for sexual favors;
(b) Use health care information to contact the patient, client or key party for the purpose of engaging in sexual misconduct;
(c) Use health care information or access to health care information to meet or attempt to meet the health care provider's sexual needs.
(4) A health care provider shall not engage, or attempt to engage, in the activities listed in subsection (1) of this section with a former patient, client or key party within two years after the provider-patient/client relationship ends.
(5) After the two-year period of time described in subsection (4) of this section, a health care provider shall not engage, or attempt to engage, in the activities listed in subsection (1) of this section if:
(a) There is a significant likelihood that the patient, client or key party will seek or require additional services from the health care provider; or
(b) There is an imbalance of power, influence, opportunity and/or special knowledge of the professional relationship.
(6) When evaluating whether a health care provider is prohibited from engaging, or attempting to engage, in sexual misconduct, the secretary will consider factors, including but not limited to:
(a) Documentation of a formal termination and the circumstances of termination of the provider-patient relationship;
(b) Transfer of care to another health care provider;
(c) Duration of the provider-patient relationship;
(d) Amount of time that has passed since the last health care services to the patient or client;
(e) Communication between the health care provider and the patient or client between the last health care services rendered and commencement of the personal relationship;
(f) Extent to which the patient's or client's personal or private information was shared with the health care provider;
(g) Nature of the patient or client's health condition during and since the professional relationship;
(h) The patient or client's emotional dependence and vulnerability; and
(i) Normal revisit cycle for the profession and service.
(7) Patient, client or key party initiation or consent does not excuse or negate the health care provider's responsibility.
(8) These rules do not prohibit:
(a) Providing health care services in case of emergency where the services cannot or will not be provided by another health care provider;
(b) Contact that is necessary for a legitimate health care purpose and that meets the standard of care appropriate to that profession; or
(c) Providing health care services for a legitimate health care purpose to a person who is in a preexisting, established personal relationship with the health care provider where there is no evidence of, or potential for, exploiting the patient or client.
[Statutory Authority: RCW 18.130.050, 18.130.062, and Executive Order 06-03. WSR 15-24-087, § 246-16-100, filed 11/30/15, effective 12/31/15. Statutory Authority: RCW 18.130.050 (1), (12) and 18.130.180. WSR 06-18-045, § 246-16-100, filed 8/30/06, effective 9/30/06.]
MANDATORY REPORTING
PDF246-16-200
Mandatory reporting—Intent.
These mandatory reporting rules require certain reports about license holders and are intended to address patient safety. These rules are not intended to limit reports from any person who has a concern about a license holder's conduct or ability to practice safely.
[Statutory Authority: RCW 18.130.070 and 18.130.060. WSR 08-08-066, § 246-16-200, filed 3/31/08, effective 5/1/08.]
PDF246-16-210
Mandatory reporting—Definitions.
(1) "Approved impaired practitioner or voluntary substance abuse program" means a program authorized by RCW 18.130.175 and approved by a disciplining authority listed in RCW 18.130.040.
(2) "Conviction" means a court has decided a person is guilty of any gross misdemeanor or felony. It includes any guilty or no contest plea and all decisions with a deferred or suspended sentence.
(3) "Determination or finding" means a final decision by an entity required or requested to report under this chapter. This applies even if no adverse action or sanction has been imposed or if the license holder is appealing the decision.
(4) "License holder" means a person holding a credential in a profession regulated by a disciplining authority listed in RCW 18.130.040(2).
(5) "Unable to practice with reasonable skill and safety due to a mental or physical condition" means a license holder who:
(a) A court has declared to be incompetent or mentally ill; or
(b) Is not successfully managing a mental or physical condition and as a result poses a risk to patient safety.
(6) "Unprofessional conduct" means the acts, conduct, or conditions described in RCW 18.130.180.
[Statutory Authority: RCW 18.130.070 and 18.130.060. WSR 08-08-066, § 246-16-210, filed 3/31/08, effective 5/1/08.]
PDF246-16-220
Mandatory reporting—How and when to report.
(1) Reports are submitted to the department of health. The department will give the report to the appropriate disciplining authority for review, possible investigation, and further action.
(a) When a patient has been harmed, a report to the department is required. A report to one of the approved impaired practitioner or voluntary substance abuse programs is not a substitute for reporting to the department.
(b) When there is no patient harm, reports of inability to practice with reasonable skill and safety due to a mental or physical condition may be submitted to one of the approved impaired practitioner or voluntary substance abuse programs or to the department. Reports of unprofessional conduct are submitted to the department.
(c) Reports to a national practitioner data bank do not meet the requirement of this section.
(2) The report must include enough information to enable the disciplining authority to assess the report. If these details are known, the report should include:
(a) The name, address, and telephone number of the person making the report.
(b) The name, address, and telephone number(s) of the license holder being reported.
(c) Identification of any patient or client who was harmed or placed at risk.
(d) A brief description or summary of the facts that caused the report, including dates.
(e) If court action is involved, the name of the court, the date of filing, and the docket number.
(f) Any other information that helps explain the situation.
(3) Reports must be submitted no later than thirty calendar days after the reporting person has actual knowledge of the information that must be reported.
[Statutory Authority: RCW 18.130.070 and 18.130.060. WSR 08-08-066, § 246-16-220, filed 3/31/08, effective 5/1/08.]
PDF246-16-230
Mandatory reporting—License holder self reports.
Each license holder must self report:
(1) Any conviction, determination, or finding that he or she has committed unprofessional conduct; or
(2) Information that he or she is unable to practice with reasonable skill and safety due to a mental or physical condition; or
(3) Any disqualification from participation in the federal medicare or medicaid program.
[Statutory Authority: RCW 18.130.070 and 18.130.060. WSR 08-08-066, § 246-16-230, filed 3/31/08, effective 5/1/08.]
PDF246-16-235
Mandatory reporting—License holder reporting other license holders.
A license holder must report another license holder in some circumstances.
(1) The reporting license holder must submit a report when he or she has actual knowledge of:
(a) Any conviction, determination, or finding that another license holder has committed an act that constitutes unprofessional conduct; or
(b) That another license holder may not be able to practice his or her profession with reasonable skill and safety due to a mental or physical condition.
(2) The license holder does not have to report when he or she is:
(a) A member of a professional review organization as provided in WAC 246-16-255;
(b) Providing health care to the other license holder and the other license holder does not pose a clear and present danger to patients or clients; or
(c) Part of a federally funded substance abuse program or approved impaired practitioner or voluntary substance abuse program and the other license holder is participating in treatment and does not pose a clear and present danger to patients or clients.
[Statutory Authority: RCW 18.130.070 and 18.130.060. WSR 08-08-066, § 246-16-235, filed 3/31/08, effective 5/1/08.]
PDF246-16-240
Mandatory reporting—Reports by professional liability insurance carriers.
Every institution, corporation or organization providing professional liability insurance to a license holder must report:
(1) Any malpractice settlement, award, or payment in excess of twenty thousand dollars that results from a claim or action for damages allegedly caused by a license holder's incompetence or negligence in the practice of the profession.
(2) Award, settlement, or payment of three or more claims during a twelve-month period that result from claims or actions for damages allegedly caused by the license holder's incompetence or negligence in the practice of the profession.
[Statutory Authority: RCW 18.130.070 and 18.130.060. WSR 08-08-066, § 246-16-240, filed 3/31/08, effective 5/1/08.]
PDF246-16-245
Mandatory reporting—Reports by health care institutions.
(1) This section applies to:
(a) Hospitals and specialty hospital defined in chapter 70.41 RCW;
(b) Ambulatory surgery facilities defined in chapter 70.230 RCW;
(c) Childbirth centers defined in chapter 18.46 RCW;
(d) Nursing homes defined in chapter 18.51 RCW;
(e) Chemical dependency treatment programs defined in chapter 70.96A RCW;
(f) Drug treatment agencies defined in chapter 69.54 RCW; and
(2) The chief administrator or executive officer or designee of these institutions must report when:
(a) A license holder's services are terminated or restricted because a license holder has harmed or placed at unreasonable risk of harm a patient or client; or
(b) A license holder poses an unreasonable risk of harm to patients or clients due to a mental or physical condition.
(3) Reports made by a hospital according to RCW 70.41.210 meet the requirement.
(4) Commencing July 1, 2009, reports made by an ambulatory surgical center according to RCW 70.230.110 meet the requirement.
[Statutory Authority: RCW 18.130.070 and 18.130.060. WSR 08-08-066, § 246-16-245, filed 3/31/08, effective 5/1/08.]
PDF246-16-250
Mandatory reporting—Reports by health service contractors and disability insurers.
[Statutory Authority: RCW 18.130.070 and 18.130.060. WSR 08-08-066, § 246-16-250, filed 3/31/08, effective 5/1/08.]
PDF246-16-255
Mandatory reporting—Reports by professional review organizations.
(1) This section applies to every peer review committee, quality improvement committee, or other similarly designated professional review organization operating in the state of Washington.
(2) Unless prohibited by state or federal law, the professional review organization must report:
(a) When it makes a determination or finding that a license holder has caused harm to a patient or placed a patient at unreasonable risk of harm; and
(b) When it has actual knowledge that the license holder poses an unreasonable risk of harm due to a mental or physical condition.
(3) Professional review organizations and individual license holders participating in a professional review organization do not need to report during the investigative phase of the professional review organization's operation if the organization completes the investigation in a timely manner.
[Statutory Authority: RCW 18.130.070 and 18.130.060. WSR 08-08-066, § 246-16-255, filed 3/31/08, effective 5/1/08.]
PDF246-16-260
Mandatory reporting—Reports by courts.
The department requests that the clerks of trial courts in Washington report professional malpractice judgments and all convictions against a license holder.
[Statutory Authority: RCW 18.130.070 and 18.130.060. WSR 08-08-066, § 246-16-260, filed 3/31/08, effective 5/1/08.]
PDF246-16-265
Mandatory reporting—Reports by state and federal agencies.
The department requests that any state or federal program employing a license holder in Washington reports:
(1) When it determines a license holder has harmed or placed at unreasonable risk of harm a patient or client; and
(2) When it has actual knowledge that the license holder poses an unreasonable risk of harm due to a mental or physical condition.
[Statutory Authority: RCW 18.130.070 and 18.130.060. WSR 08-08-066, § 246-16-265, filed 3/31/08, effective 5/1/08.]
PDF246-16-270
Mandatory reporting—Reports by employers of license holders.
(1) Every license holder, corporation, organization, health care facility, and state and local governmental agency that employs a license holder shall report to the department of health when the employed license holder's services have been terminated or restricted based on a final determination or finding that the license holder:
(a) Has committed an act or acts that may constitute unprofessional conduct; or
(b) May not be able to practice his or her profession with reasonable skill and safety due to a mental or physical condition.
(2) Reports under this section must be submitted to the department of health as soon as possible but no later than twenty days after a final determination or finding is made. The report should contain the information described in WAC 246-16-220(2).
(3) Reports made by a hospital according to RCW 70.41.210 and reports by ambulatory surgical facilities according to RCW 70.230.120 meet the requirement of this section.
(4) If a license holder fails to submit a report required by this section, a civil penalty of up to five hundred dollars may be imposed and the disciplining authority may take action against the license holder for unprofessional conduct.
[Statutory Authority: RCW 18.130.080. WSR 09-04-050, § 246-16-270, filed 1/30/09, effective 3/2/09.]
SANCTIONS
PDF246-16-800
Sanctions—General provisions.
(1) Applying these rules.
(a) The disciplining authorities listed in RCW 18.130.040(2) will apply these rules to determine sanctions imposed for unprofessional conduct by a license holder in any active, inactive, or expired status. The rules do not apply to applicants.
(b) The disciplining authorities will apply the rules in:
(i) Orders under RCW 18.130.110 or 18.130.160; and
(ii) Stipulations to informal disposition under RCW 18.130.172.
(c) Sanctions will begin on the effective date of the order.
(2) Selecting sanctions.
(a) The disciplining authority will select sanctions to protect the public and, if possible, rehabilitate the license holder.
(b) The disciplining authority may impose the full range of sanctions listed in RCW 18.130.160 for orders and RCW 18.130.172 for stipulations to informal dispositions.
(i) Suspension or revocation will be imposed when the license holder cannot practice with reasonable skill or safety.
(ii) Permanent revocation may be imposed when the disciplining authority finds the license holder can never be rehabilitated or can never regain the ability to practice safely.
(iii) Surrender of a credential may be imposed when the license holder is at the end of his or her effective practice and surrender alone is enough to protect the public. The license holder must agree to retire and not resume practice.
(iv) Indefinite suspension may be imposed in default and waiver of hearing orders. If indefinite suspension is not imposed in a default or waiver of hearing order, the disciplining authority shall impose sanctions determined according to these rules.
(v) "Oversight" means a period of time during which respondent must engage in on-going affirmative conduct intended to encourage rehabilitation and ensure public safety. It also includes active compliance monitoring by the disciplining authority. The passage of time without additional complaints or violations, with or without payment of a fine or costs, is not, by itself, oversight.
(c) The disciplining authority may deviate from the sanction schedules in these rules if the schedule does not adequately address the facts in a case. The disciplining authority will acknowledge the deviation and state its reasons for deviating from the sanction schedules in the order or stipulation to informal disposition.
(d) If the unprofessional conduct is not described in a schedule, the disciplining authority will use its judgment to determine appropriate sanctions. The disciplining authority will state in the order or stipulation to informal disposition that no sanction schedule applies.
(3) Using sanction schedules.
(a) Step 1: The findings of fact in an order or the allegations in an informal disposition describe the unprofessional conduct. The disciplining authority uses the unprofessional conduct described to select the appropriate sanction schedule contained in WAC 246-16-810 through 246-16-860.
(i) If the act of unprofessional conduct falls in more than one sanction schedule, the greater sanction is imposed.
(ii) If different acts of unprofessional conduct fall in the same sanction schedule, the highest sanction is imposed and the other acts of unprofessional conduct are considered aggravating factors.
(b) Step 2: The disciplining authority identifies the severity of the unprofessional conduct and identifies a tier using the sanction schedule tier descriptions.
(c) Step 3: The disciplining authority identifies aggravating or mitigating factors using the list in WAC 246-16-890. The disciplining authority describes the factors in the order or stipulation to informal disposition.
(d) Step 4: The disciplining authority selects sanctions within the identified tier. The starting point for duration of the sanctions is the middle of the tier range.
(i) Aggravating factors move the appropriate sanctions towards the maximum end of the tier range.
(ii) Mitigating factors move the appropriate sanctions towards the minimum end of the tier range.
(iii) Mitigating or aggravating factors may result in determination of a sanction outside the range in the tier. The disciplining authority will state its reasons for deviating from the tier range in the sanction schedule in the order or stipulation to informal disposition. The disciplining authority has complied with these rules if it acknowledges the deviation and states its reasons for deviating from the sanction schedules in the order or stipulation to informal disposition.
[Statutory Authority: RCW 18.130.390. WSR 09-15-190, § 246-16-800, filed 7/22/09, effective 8/22/09.]
PDF246-16-810
Sanction schedule—Practice below standard of care.
 |
[Statutory Authority: RCW 18.130.390. WSR 09-15-190, § 246-16-810, filed 7/22/09, effective 8/22/09.]
PDF246-16-820
Sanction schedule—Sexual misconduct or contact.
 |
[Statutory Authority: RCW 18.130.390. WSR 09-15-190, § 246-16-820, filed 7/22/09, effective 8/22/09.]
PDF246-16-830
Sanction schedule—Abuse—Physical and emotional.
 |
[Statutory Authority: RCW 18.130.390. WSR 09-15-190, § 246-16-830, filed 7/22/09, effective 8/22/09.]
PDF246-16-840
Sanction schedule—Diversion of controlled substances or legend drugs.
 |
[Statutory Authority: RCW 18.130.390. WSR 09-15-190, § 246-16-840, filed 7/22/09, effective 8/22/09.]
PDF246-16-850
Sanction schedule—Substance abuse.
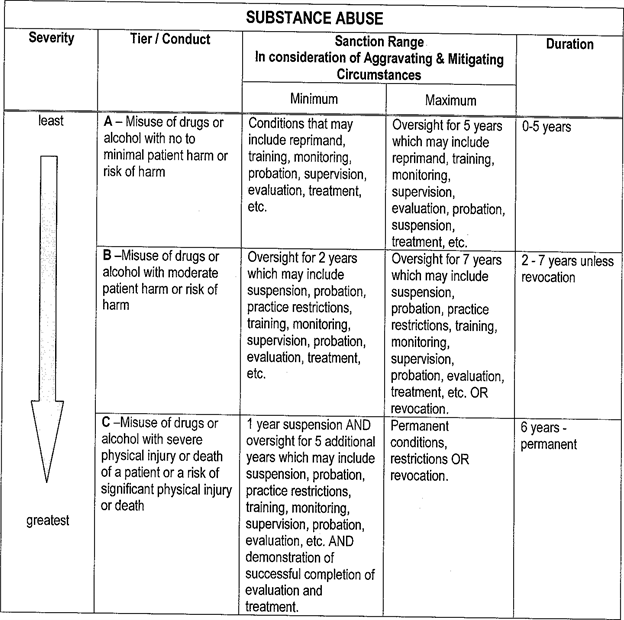 |
[Statutory Authority: RCW 18.130.390. WSR 09-15-190, § 246-16-850, filed 7/22/09, effective 8/22/09.]
PDF246-16-860
Sanction schedule—Criminal convictions.
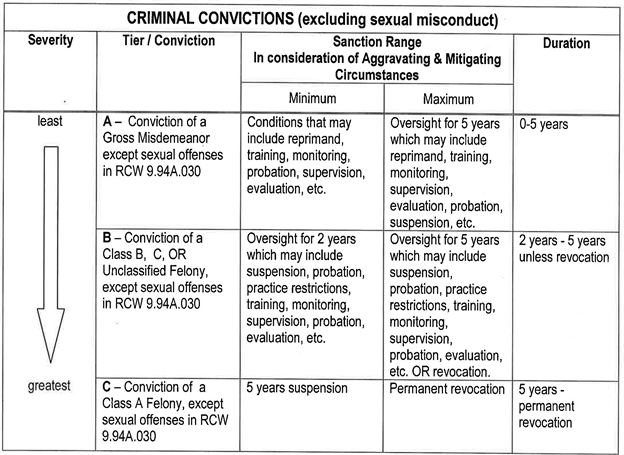 |
[Statutory Authority: RCW 18.130.390. WSR 09-15-190, § 246-16-860, filed 7/22/09, effective 8/22/09.]
PDF246-16-890
Sanctions—Aggravating and mitigating factors.
The following nonexclusive list identifies factors that may mitigate or aggravate the sanctions that should be imposed in an order or stipulation to informal disposition.
(1) Factors related to the unprofessional conduct:
(a) Gravity of the unprofessional conduct;
(b) Age, capacity and/or vulnerability of the patient, client or victim;
(c) Number or frequency of the acts of unprofessional conduct;
(d) Injury caused by the unprofessional conduct;
(e) Potential for injury to be caused by the unprofessional conduct;
(f) Degree of responsibility for the outcome;
(g) Abuse of trust;
(h) Intentional or inadvertent act(s);
(i) Motivation is criminal, immoral, dishonest or for personal gain;
(j) Length of time since the unprofessional conduct occurred.
(2) Factors related to the license holder:
(a) Experience in practice;
(b) Past disciplinary record;
(c) Previous character;
(d) Mental and/or physical health;
(e) Personal circumstances;
(f) Personal problems having a nexus with the unprofessional conduct.
(3) Factors related to the disciplinary process:
(a) Admission of key facts;
(b) Full and free disclosure to the disciplining authority;
(c) Voluntary restitution or other remedial action;
(d) Bad faith obstruction of the investigation or discipline process or proceedings;
(e) False evidence, statements or deceptive practices during the investigation or discipline process or proceedings;
(f) Remorse or awareness that the conduct was wrong;
(g) Impact on the patient, client, or victim.
(4) General factors:
(a) License holder's knowledge, intent, and degree of responsibility;
(b) Presence or pattern of other violations;
(c) Present moral fitness of the license holder;
(d) Potential for successful rehabilitation;
(e) Present competence to practice;
(f) Dishonest or selfish motives;
(g) Illegal conduct;
(h) Heinousness of the unprofessional conduct;
(i) Ill repute upon the profession;
(j) Isolated incident unlikely to reoccur.
[Statutory Authority: RCW 18.130.390. WSR 09-15-190, § 246-16-890, filed 7/22/09, effective 8/22/09.]